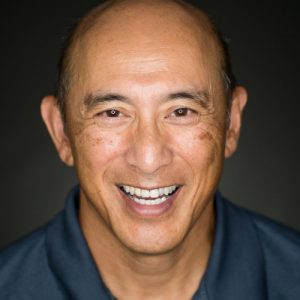
Gene has a 30+ year career building health care businesses, focusing on health services companies, health plans, provider organizations and most recently payment reform and value-based care initiatives. Gene managed home health care and home IV therapy businesses, was chief operating officer of OptiCare Eye Health and was president and chief development officer of a multi-state physician home visit company that was sold to CIGNA.
In the health plan sector, he built the Medicare Advantage business from startup to an $850 million unit of Oxford Health Plans in the CT/NY/NJ market, was CEO of Citrus HealthCare in Tampa in a turnaround/ownership transition, ran the Medicare Advantage plan for HealthNet of the Northeast, built Chronic Special Needs Plans for Aveta and ran the nationwide 24-hour nurse line for IntraCorp/CIGNA HealthCare. From 2013 to 2018, Gene led the post-acute business for Remedy Partners, the largest player in the CMS Bundled Payment for Care Improvement program, generating substantial savings for Medicare, surpluses for SNF partners and returns for investors.
Gene has been on the ReferWell Board since 2015 and in his role as executive chairman, works on behalf of the Board with the CEO and his team to develop significant payer relationships and key strategic partnerships to maximize enterprise value. Gene holds a bachelor’s degree in chemistry from Cornell University and Master’s in the Management of Technology from Massachusetts Institute of Technology.